Introduction
Twenty-two years – it is staggering. The average life expectancy of a police officer in the United States is twenty-two years less than their civilian counterparts.[1] As a police officer, life expectancy is only 57 years, compared to 69 years in the civilian sector. This, however, is just the tip of the iceberg.[2]
A newly sworn officer who has just graduated the police academy is most often in the best physical shape of his or her life. That young officer has also undergone and passed a psychological screening assessment and is has been determined to be in good mental health as well. The tragedy is that over the next twenty to twenty five years of their careers, these officers will suffer physical illness and emotional trauma with devastating consequence. When compared to their civilian counterparts, law enforcement officers not only have a shorter life expectancy, but higher rates of heart disease, hypertension, diabetes and obesity. A career in in policing is also associated with increased rates of mental health issues which results in higher frequency of divorce, substance and alcohol abuse and suicide.
Because of disparity of physical and mental health issues that is seen in law enforcement officers nationwide, it is the absolute duty of command staff to ensure that the officers under their watch not only go home at the end of their shift, but also stay physically and mentally healthy. A young officer in the early stages of his or her career is a phenomenal “raw material”. The protection of these individuals goes well beyond policy directives regarding items such as the wearing body armor and reflective vests etc. It requires a comprehensive approach to wellness, allowing them a productive and fulfilling career and the ability to enjoy the retirement for which they have worked so hard.
The question of “what is wellness” can be answered in a myriad of ways and is usually defined by the background of the individual asking the question. Psychologists often see wellness in terms of mental health and resiliency. The chaplaincy corps will define a specific type of spiritual wellness and medical professionals will often determine wellness as the absence of a specific state of disease or illness. All these professionals are correct, as an effective wellness initiative does require a multidisciplinary approach
Over the last several years, multiple organizations including the United States Department of Justice, the International Association of Chiefs of Police, the National Law Enforcement Memorial Fund, Below One Hundred, The Institute for Intergovernmental Research and the Officer Down Memorial Page (to name just a few) have done a tremendous job in identifying the scope of increased officer morbidity and mortality. These organizations have developed multiple initiatives to address these issues and significant progress has been made, but there is still work to be done.
Regardless of the forum, there are consistently five areas of wellness that are repeatedly discussed: tactical combat casualty care, cardiac screening, physical fitness, maintenance of a healthy weight and mental health. It should be noted that physical fitness and healthy weight management overlap but are distinctly different entities. It is not unusual for an individual to be overweight but fit, or conversely, of normal weight and not fit. Every wellness program, no matter what its scope, addresses these specific issues at some level.
Tactical combat casualty care
The concept of a wellness initiative must consider one of the fundamental problems that law enforcement officers may face, the possibility of traumatic injury. Over the last several years, tremendous strides have been made to address this issue. The proliferation of advanced trauma care within both the law enforcement and civilian community has its origins in the aftermath of mass casualty events. The medical technology developed during military operations over the last twenty years has resulted in the proliferation of next generation tourniquets, hemostatic gauze, and tools to manage airways and chest wall injuries.
It is obvious that law enforcement officers must have the tools and training to provide lifesaving trauma care to themselves and to their fellow officers. It is therefore vital that officers are equipped and trained appropriately. The development of belt mounted tourniquet systems ensure that officers have a tourniquet available at every possible moment (figure 1). A readily available tourniquet prevents an officer from having to retrieve this piece of equipment when injured. There are countless examples of officers who are injured during the line of duty and are able to self-apply a tourniquet, stopping their hemorrhage and allowing them to not only survive the encounter but to “stay in the fight.” It has also been universally recognized that a standard issue individual first aid kit (IFAK) is just as vital. An IFAK which contains hemostatic gauze, a standard pressure dressing and an occlusive chest wall seal gives officers the absolute best chance of providing self-aid and buddy aid during any type of traumatic injury.
Standardized issue, in which all officers carry the same equipment is also vital. During a critical incident in which an officer is injured several compounding circumstances are present. There is usually low light, the officer’s hands are frequently wet with either blood or sweat and due to the increased adrenaline release, there is loss of fine motor control and possibly the development of tunnel vision. In this situation the ability to reproduce a particular movement without conscious thought or “muscle memory” is vital. The use of an unfamiliar piece of equipment may result in ineffective application and subsequent inability to successfully treat an injury. Standardization also allows officers the ability to share equipment in an emergency in the same way pistol magazines can be shared if the same weapon platform is used.
There is also an obvious need for initial and continued training in tactical first aid. The development of initial training and familiarization with the issued equipment must be reinforced with annual refresher training. Officers should also be required by policy to carry their trauma gear in a standard location. Tourniquets should be belt mounted and IFAKS should be either on the officer or mounted to specified area in the patrol car. In a critical incident an officer’s medical gear must be easily found by rescuing fellow officers. With standardized issue, standardized training and standardized carry, the chance of an officer succumbing to a traumatic injury is significantly minimized.

Cardiac screening
There is no question that one of the top killers of men and women in uniform is heart disease. Although death from heart attack is consistently ranked as the number two or three cause of death by tracking organizations such as the Officer Down Memorial Page (ODMP)[3], or the National Law Enforcement Officer Memorial Fund (NLEOMF)[4], these rankings do not include heart attack deaths that occur after the individual officer finishes the duty shift. When these numbers are extrapolated for a twenty-four-hour day, heart attack easily becomes the number one killer of men and women in uniform. Furthermore, it is well known that less than 3% of heart attacks are fatal [5], meaning the published data doesn’t capture and recognize literally the thousands of heart attacks that result in significant officer disability but do not result in death. Besides the toll on human life, heart attacks are one of the leading medical expenses that police agencies must face. According to The Commission on Accreditation for Law Enforcement Agencies (CALEA), the cost to the taxpayers of an in service heart attack ranges from $450k to $750k per incident.
According to data published the average age of a US police officer who suffers a heart attack is 46 year, while the average age of a civilian is 65 years[6]. More striking is that a civilian who is between the ages of 55 and 59 has only 1.5 % chance of dying from a heart attack, while police officers in the same age range have a chance of over 56%[7] More frequent heart attacks which occur at younger ages contribute to that horrific statistic of police officers having life expectancy that is 22 years less than their civilian counterparts. Despite the fact that police officers are twenty-five times more likely to die from a cardiovascular event (i.e. heart attack or stroke) than be killed by the violent action of a suspect, little information regarding this significant problem has been adequately disseminated to executive leadership and to line officers as well[8].
The cause of increased cardiac risk in policing remains elusive but is likely related not only to an increased prevalence of known classic risk factors (hypertension, high cholesterol, diabetes etc.) but also to factors such as mental stress induced by work schedules, shift work, hypervigilance and psychological trauma.
Law enforcement is certainly a stressful profession, but it is not unique in this regard. Stress is absolutely ubiquitous in our society. However, police officers are known to have a stress pattern which is unique and very different than what is seen in individuals in the civilian sector. In data from more than 4,500 US LEOs from 1984 to 2010, it was found risk of sudden cardiac death was 34-69 times higher during restraints and altercations, 32-51 times higher during pursuits, 20-23 times higher during physical training, and 6-9 times higher during medical/rescue operations.” [9]
The inherent nature of policing consists of long periods of routine and sometimes mundane patrol or investigation punctuated by short periods intense excitement which results in accelerated adrenaline release. This is the so-called pattern of policing which is often described as “98% boredom and 2% sheer terror.” This unexpected and rapid secretion in adrenaline results in several rapid physiological changes. Initially, there is a sudden increase in heart rate and blood pressure. There is repeated Valsalva maneuver (increased intrathoracic pressure from breath holding and bearing down), as well as activation of both the left and right hemispheres of the brain as the officer use both sides of his or her upper and lower body in offensive and defensive threat mitigation. These intense episodes may go on for several minutes, and in many cases when officers are “fighting for their lives” they will rapidly convert from aerobic to anaerobic metabolism.[10]
It is also known that heart attacks resulting from these described changes in physiology, will often happen hours after the instigating event. Several states recognize this delay and therefore presumptively consider any law enforcement officer who suffers a cardiac issue while off duty to have developed the initial stages of their event while on duty.
A strategy to prevent heart attacks requires understanding of the simple pathophysiology of how these events occur. A heart attack, or myocardial infarction (MI) occurs when one of the coronary arteries that supplies the heart is blocked. A blocked coronary artery does not occur from a gradual narrowing of the blood vessel. In other words, a blocked or occluded artery does not block slowly over time.
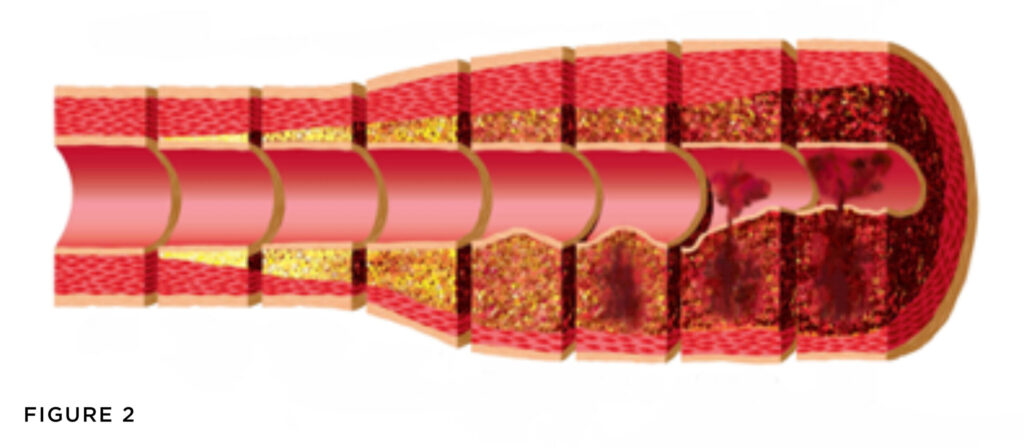
When plaque or blockage begins to form in an artery, it does not form in the interior or what is known as lumen of the artery such as scale would in a pipe. Instead, plaque accumulates in the actual wall of the blood vessel (figure 2). As the plaque begins to accumulate inside the arterial wall, the artery will become inflamed. This inflammation will eventually become so severe, that the plaque in the artery will burst or rupture causing the plaque to spill out from the wall of the blood vessel into the opening of the artery. This plaque rupture causes the clotting system to activate forming a 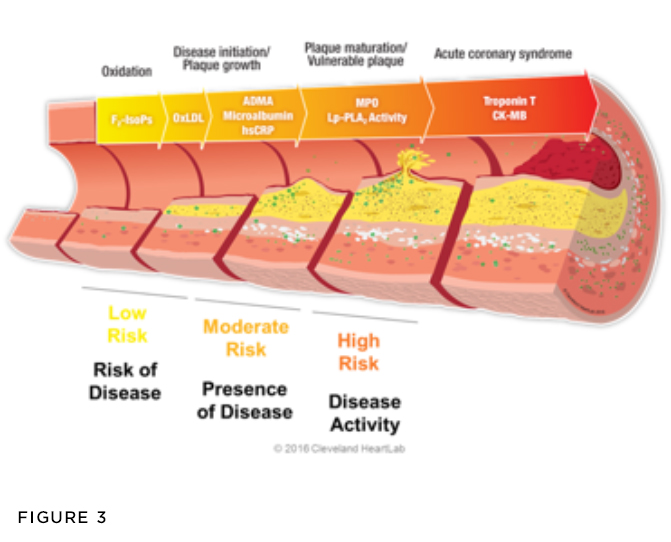 clot within the artery. This clot immediately blocks blood flow. (figure 3). Current thought is that the unique stress pattern seen in law enforcement can potentially accelerate plaque rupture which results in the increase frequency of heart attacks.
clot within the artery. This clot immediately blocks blood flow. (figure 3). Current thought is that the unique stress pattern seen in law enforcement can potentially accelerate plaque rupture which results in the increase frequency of heart attacks.
Because of advanced understanding of the pathophysiology of heart attacks, the concept that heart attacks occur without warning is truly antiquated. There are specific tests that can detect the presence of blockages or coronary artery disease (CAD), years before these blockages cause symptoms. Standard stress testing, such as exercise treadmill testing, or bicycle stress testing will only detect blockages which are already significant enough to obstruct blood flow. This testing will not detect mild plaque or blockages in their very early stages. For this, more advanced yet simple alternative tests are needed.
When the early stages of plaque forms within the artery wall, several things occur that can be detected before plaque ruptures and a heart attack occurs. A very low dose radiation computed tomography (CT or CAT) scan known as a coronary artery calcium (CAC) scan is able to detect little “flecks” of calcium which develop within the coronary arteries (figures 4 and 5). This scan typically costs less than $100, uses a low dose of radiation (0.7 mSv) and can be done in a matter of minutes. More predictive than coronary calcium scoring, is the ability to detect inflammatory changes within the artery by measuring certain biomarkers seen on specific blood tests. Markers such as oxidized LDL (OXLDL), myeloperoxidase (MPO), asymmetric dimethyl arginine (ADMA) and lipoprotein associated phospholipase A2 (Lp-Pla2) can identify inflamed plaque and provide evidence that the plaque is prone to rupture. Of these markers, the most studied and most predictive is Lp-Pla2. When this specific marker is elevated, the risk of that individual having plaque rupture and therefore a heart attack is approximately 15-20% over a 4 year period of time[11].
 From a pragmaic standpoint, the combination calcium scoring and Lp-PLA2 detection is extremely useful in detecting coronary disease years before a heart attack occurs. After studying over 3800 police officers without any symptoms of heart disease, 31% were found to have a positive calcium score, 26% were found to have an elevation of Lp-Pla2, but only 7% had both markers – making the need to evaluate both these tests invaluable. Shockingly, this data clearly demonstrates that of the 3836 officers screened, 64% had evidence of undiagnosed coronary artery disease.[12] Disease that can be identified and successfully treated resulting in fewer officers succumbing to heart attacks and becoming statistics.
From a pragmaic standpoint, the combination calcium scoring and Lp-PLA2 detection is extremely useful in detecting coronary disease years before a heart attack occurs. After studying over 3800 police officers without any symptoms of heart disease, 31% were found to have a positive calcium score, 26% were found to have an elevation of Lp-Pla2, but only 7% had both markers – making the need to evaluate both these tests invaluable. Shockingly, this data clearly demonstrates that of the 3836 officers screened, 64% had evidence of undiagnosed coronary artery disease.[12] Disease that can be identified and successfully treated resulting in fewer officers succumbing to heart attacks and becoming statistics.
Once detected, coronary disease can be mitigated, and risk of heart attack can be significantly reduced. There is a well identified three pronged approach to reducing risk. First, certain cholesterol medications, particularly the HMG co-reductase inhibitors or “statins” have been definitively proven to cause plaque to regress and to reduce coronary inflammation.[13] Secondly, changes in lifestyle, specifically changes in diet and exercise patterns have also been shown to not only reduce coronary disease, but to prolong life and reduce metabolic issues such as obesity, hypertension and diabetes. Finally, the use of certain nutritional supplements has also been shown to reduce risk in specific populations. For example, in those individuals who have an elevation of Lp-Pla2, one of the components of fish oil, known as icosapent ethyl, or EPA has been successfully shown to significantly reduce inflammation.[14] Heart attack is preventable and does not have to be one of the top killers of men and women in uniform. It can be detected early, and once identified; it can be successfully treated.
 Fitness
Fitness
There is no question that being a police officer requires a level of fitness that is not needed in other professions. It has been proven time and again, that individuals who exercise live longer than those that do not.[15] High density lipoprotein (HDL) or “good cholesterol” is the cholesterol molecule that is responsible for reverse cholesterol transport, that is, it is the molecule that effectively absorbs plaque from the arterial wall and returns it to the liver for destruction. Aerobic exercise has been shown not only to increase the amount of HDL in the blood, but exercise also increases the HDL size and improves its ability to clear plaque.[16]
Police officers have also been shown to have potential exposure to excessive liability if they are not fit. At times, an unfit police officer does not have the ability to go “hands on” with an assailant and may have a higher likelihood to resort to lethal force. In a landmark trial, Parker v District of Columbia, a Metropolitan police officer was found that due to his physical condition, “…it is not hard to fathom that his most effective method for subduing the objects of his pursuits would be the use of a firearm as opposed to the application of physical force…“Furthermore, the District was found liable as, “…Officer Hayes simply was not in adequate physical shape. This condition posed a foreseeable risk of harm to others. We are persuaded that a fair-minded jury could have concluded that Officer Hayes’ conduct was the result of deliberate indifference on the part of the District with respect to the physical training of its police officers…”[17].
Finally, the Federal Bureau of Investigation Behavioral Science Unit found that officers who appeared unfit were more likely to face physical resistance and assault than officers who appeared fit[18]. This information was so compelling, it has resulted in the Texas Department of Public Safety to develop the Command Presence Directive requiring both male and female officers to have acceptable waist circumference measurements.
With this data, it is imperative that officers maintain fitness throughout their careers. This appropriate mindset needs to be forged during initial training during academy instruction. Physical fitness should not be used as a punishment, the cliché of “drop and give me twenty” only associates a negative connotation with exercise. Upon graduation, young officers should have the expectation that they will need to continue to meet fitness standards in the same way that they will need to continue to meet qualification standards with duty weapons, speed measurement devices, intoxilyzers etc.
There are multiple fitness modalities that can be utilized to measure officer fitness. They range from standard physical fitness testing found in the Armed Forces using pushups, pull-ups, and a timed run, to agility courses to using novel assessments such as a stationary rower. Regardless of what type of testing is developed, adherence to standards with rewards for meeting standards and consequences for failing to meet standards need to be recognized and followed. For example, certain police departments offer a monthly cash incentive and reward a ribbon for exceeding fitness standards. Those failing to meet standards will often require remediation, retesting and can ultimately lead to noncritical job placement and even fitness for duty assessment.
Nutrition and maintenance of a healthy weight
Obesity and its consequences are also a tremendous problem among the men and women who wear the uniform. According to published data, over 80% of law enforcement officers are overweight and 40% are clinically obese[19]. In data collected by the Public Safety Cardiac Foundation, over 80% of police officers in central Texas were found to be obese[20] by body fat measurement.
Obesity often results in a myriad of comorbidities including increased rates of hypertension, diabetes as well as the development of more frequent musculoskeletal injuries. Overweight police officers can also be less effective at their jobs and may the focus of more physical resistance and potential assault. It is therefore absolutely vital that there is an expectation not only for officers to remain physically fit, but to have effective command presence.
It has been well documented through many published studies that weight loss and the maintenance of a healthy body mass cannot be achieved by exercise alone.[21] [22] [23]
There are several different diets that have been popularized over the last twenty years. Regardless of the diet, most nutrition plans will fit into one of three categories: reduced fat, reduced carbohydrate and reduced calorie. When these different approaches are comparatively studied, they all seem to be equally effective for weight reduction. [24]
From a cardiovascular standpoint, a diet that limits carbohydrates and eliminates sugar has been shown to be highly effective at reducing heart attack risk as it reduces the most destructive cholesterol particles. Low density lipoprotein (LDL) or “bad” cholesterol is the cholesterol molecule that is responsible for causing plaque formation within the artery wall. LDL exists in several sizes and densities from small dense particle to large fluffy and buoyant particles (think golf balls to beach balls) (figure 6). The small dense particles have the ability to burrow into the blood vessel wall at a much higher frequency than the large buoyant particles. When a diet which is high in carbohydrates and sugar is consumed, the liver forms more of the smaller and denser LDL particles which in turn lead to more plaque deposition. When a diet higher in fat is consumed, the liver forms larger and more buoyant particles which do not contribute to plaque formation as easily as the larger and less dense particles cannot cross the lining of the blood vessel wall.
In the 1970’s the McGovern Commission postulated that dietary fat increases LDL, LDL causes heart disease therefore dietary fat causes heart disease.[25] This has been proven inaccurate; however, the contrapositive is correct. The concept of a low fat diet being a “heart healthy” diet was very prevalent in the 1980’s 90’s. The low fat guidelines were in fact fraught with paradoxical medical outcomes. By avoiding dietary fat, Americans began to consume increasing amounts of carbohydrates. In doing so, the US entered into an obesity epidemic which resulted in increased rate of diabetes and hypertension. More concerning is the fact that the rate of cardiovascular disease did not drop, it actually increased. [26]
The diet which seems to be the most effective at minimizing heart disease and keeping obesity at bay is a diet of fresh fruits, vegetable and meat. The reduction of carbohydrates and the elimination of sugars is absolutely vital to keeping the men and women in law enforcement and the general population healthy.
Mental health
The mental health issues that plague the men and women of law enforcement are well defined. It is known the police officers suffer depression, anxiety and post-traumatic stress disorder at an increased rate as to what is seen in the civilian sector. Consequently, police officers have increased rates of divorce, substance abuse and suicide which is disproportional[27]. It is well beyond the scope of this article and the expertise of the author to address these issues other than to comment on the physical impact these issues may have.
Individuals who are under significant stress and who have not developed the proper coping mechanisms are also frequently found to be less healthy. Psychological issues can result in poor diet and poor exercise compliance. Significant stress also results in poor sleeping habits which in turn have been found to have an association not only with poor on the job performance, but increased rates of heart disease and earlier death. High levels of stress also contribute to hypertension and its associated comorbidities. It is therefore absolutely imperative that mental wellness initiatives be used in a preventative capacity, not strictly in response to crises or critical incidents.
Conclusion
A multi-disciplinary approach to officer wellness is absolutely paramount in reducing increased officer morbidity and mortality. A well designed approach to wellness must include an approach to the disproportional issues that law enforcement officer face. The development of a self-aid buddy-aid curriculum, a nutrition and exercise program, a cardiac screening initiative and comprehensive mental health policy can keep our officers alive, healthy, and more effective while on the job.
About the author
 Dr. Jonathan Sheinberg is a physician, sworn law enforcement officer and veteran. He attended Washington and Lee University before receiving his medical degree from the Georgetown University School of Medicine in Washington, DC. He completed a rotating internship at Georgetown and then completed his residency training in Internal Medicine at USAF Medical Center Keesler, located on Kessler Air Force Base, Mississippi. After residency, Dr. Sheinberg completed his fellowship in Cardiovascular Diseases at Wilford Hall USAF Medical Center, Lackland Air Force Base, Texas. He has served overseas in the United States Air Force during U.S. military operations in Haiti and in Operation Enduring Freedom.
Dr. Jonathan Sheinberg is a physician, sworn law enforcement officer and veteran. He attended Washington and Lee University before receiving his medical degree from the Georgetown University School of Medicine in Washington, DC. He completed a rotating internship at Georgetown and then completed his residency training in Internal Medicine at USAF Medical Center Keesler, located on Kessler Air Force Base, Mississippi. After residency, Dr. Sheinberg completed his fellowship in Cardiovascular Diseases at Wilford Hall USAF Medical Center, Lackland Air Force Base, Texas. He has served overseas in the United States Air Force during U.S. military operations in Haiti and in Operation Enduring Freedom.
Dr. Sheinberg has served as Assistant Professor of Medicine at Wright State University in Dayton, Ohio, and at the Uniformed Services University of the Health Sciences in Bethesda, Maryland. He currently is an associate clinical professor of medicine at the University of Texas Medical Branch, Galveston.
Besides medicine, Dr. Sheinberg’s passion is Law Enforcement. He is a licensed Peace Officer for the State of Texas, a Lieutenant on the Lakeway Police Department, and a Reserve Trooper with the Texas Department of Public Safety. He has previously served as a Special Deputy United States Marshal on the Lonestar Fugitive Taskforce.
Dr. Sheinberg has been a member of the US Dept. of Justice Presidential Task Force on 21st Century Policing and serves on the Officer Safety and Wellness Working Group. He has developed The Cardiac Screening Initiative (CSI), an observational cohort study with the intent on determining the prevalence of coronary disease in the asymptomatic law enforcement officer. He currently also serves as the Chief Medical Officer of Sigma Tactical Wellness (www.iamSigma.com) and has developed cardiac and metabolic screening programs which have been implemented in agencies throughout the United States, Canada and Europe.
During his free time, Dr. Sheinberg enjoys spending time with wife and kids. He is a military history buff and enjoys working out, playing with his dogs and traveling the country in his RV.
[1] John M. Violanti et al., “Life Expectancy in Police Officers: A Comparison with the U.S. General Population,” International Journal of Emergency Mental Health 15, no. 4 (2013): 217–28.
[2] Violanti et al.
[3] “The Officer Down Memorial Page (ODMP),” accessed December 21, 2020, https://www.odmp.org/.
[4] “Https://Nleomf.Org/,” National Law Enforcement Officers Memorial Fund, accessed December 21, 2020, https://nleomf.org/.
[5] Harvard Health Publishing, “Surviving a Heart Attack: A Success Story,” Harvard Health, accessed December 21, 2020, https://www.health.harvard.edu/heart-health/surviving-a-heart-attack-a-success-story.
[6] Violanti et al., “Life Expectancy in Police Officers.”
[7] Violanti et al.
[8] Tom Tracy, “Fit for Duty: Demand It.,” Police, March 1993, 18.
[9] Vasileia Varvarigou et al., “Law Enforcement Duties and Sudden Cardiac Death among Police Officers in United States: Case Distribution Study,” BMJ (Clinical Research Ed.) 349 (November 18, 2014): g6534, https://doi.org/10.1136/bmj.g6534.
[10] Michael E. Andrew et al., “Police Work Stressors and Cardiac Vagal Control,” American Journal of Human Biology : The Official Journal of the Human Biology Council 29, no. 5 (September 10, 2017), https://doi.org/10.1002/ajhb.22996.
[11] Emmanouil S. Brilakis et al., “Association of Lipoprotein-Associated Phospholipase A2 Levels with Coronary Artery Disease Risk Factors, Angiographic Coronary Artery Disease, and Major Adverse Events at Follow-Up,” European Heart Journal 26, no. 2 (January 1, 2005): 137–44, https://doi.org/10.1093/eurheartj/ehi010.
[12] Jonathan Sheinberg, “The Presence of Early Markers of Coroanry Artery Disease in an Asymptomatic Population of Law Enforcement Officers” (June 2020).
[13] Lima João A.C. et al., “Statin-Induced Cholesterol Lowering and Plaque Regression After 6 Months of Magnetic Resonance Imaging–Monitored Therapy,” Circulation 110, no. 16 (October 19, 2004): 2336–41, https://doi.org/10.1161/01.CIR.0000145170.22652.51.
[14] Mitsuhiro Yokoyama et al., “Effects of Eicosapentaenoic Acid on Major Coronary Events in Hypercholesterolaemic Patients (JELIS): A Randomised Open-Label, Blinded Endpoint Analysis,” The Lancet 369, no. 9567 (March 31, 2007): 1090–98, https://doi.org/10.1016/S0140-6736(07)60527-3.
[15] Peter Kokkinos, “Physical Activity, Health Benefits, and Mortality Risk,” ISRN Cardiology 2012 (October 30, 2012): 1–14, https://doi.org/10.5402/2012/718789.
[16] Jonathan J. Ruiz-Ramie, Jacob L. Barber, and Mark A. Sarzynski, “Effects of Exercise on HDL Functionality,” Current Opinion in Lipidology 30, no. 1 (February 2019): 16–23, https://doi.org/10.1097/MOL.0000000000000568.
[17] “Parker v. District of Columbia, 850 F.2d 708 | Casetext Search + Citator,” accessed December 24, 2020, https://casetext.com/case/parker-v-district-of-columbia-2.
[18] Anthony Pinizzotto, Edward Davis, and Charles Miller III, “The Deadly Mix. Officers, Offenders and the Circumstances That Bring Them Together.,” The FBI Law Enforcement Bulletin, January 2007.
[19] Daniel Shell, “The Police Executive Leadership Program Class Exercise and Nutrition Questionnaire, Division of Public Safety Leadership” (Johns Hopkins University, October 2003).
[20] Sheinberg, “The Presence of Early Markers of Coroanry Artery Disease in an Asymptomatic Population of Law Enforcement Officers.”
[21] Herman Pontzer et al., “Constrained Total Energy Expenditure and Metabolic Adaptation to Physical Activity in Adult Humans,” Current Biology26, no. 3 (February 8, 2016): 410–17, https://doi.org/10.1016/j.cub.2015.12.046.
[22] Damon L. Swift et al., “The Role of Exercise and Physical Activity in Weight Loss and Maintenance,” Progress in Cardiovascular Diseases 56, no. 4 (2014): 441–47, https://doi.org/10.1016/j.pcad.2013.09.012.
[23] Swift et al.
[24] Frank M. Sacks et al., “Comparison of Weight-Loss Diets with Different Compositions of Fat, Protein, and Carbohydrates,” New England Journal of Medicine 360, no. 9 (February 26, 2009): 859–73, https://doi.org/10.1056/NEJMoa0804748.
[25] “Dietary Goals for the United States / Prepared by the Staff of the Select Committee on Nutrition and Human Needs, United States Senate.,” n.d., 131.
[26] null null et al., “Heart Disease and Stroke Statistics—2006 Update,” Circulation 113, no. 6 (February 14, 2006): e85–151, https://doi.org/10.1161/CIRCULATIONAHA.105.171600.
[27] Miriam Heyman, Jeff Dill, and Robert Douglas, “The Ruderman White Paper On,” n.d., 41.
Sources
Andrew, Michael E., John M. Violanti, Ja K. Gu, Desta Fekedulegn, Shengqiao Li, Tara A. Hartley, Luenda E. Charles, Anna Mnatsakanova, Diane B. Miller, and Cecil M. Burchfiel. “Police Work Stressors and Cardiac Vagal Control.” American Journal of Human Biology : The Official Journal of the Human Biology Council 29, no. 5 (September 10, 2017). https://doi.org/10.1002/ajhb.22996.
Brilakis, Emmanouil S., Joseph P. McConnell, Ryan J. Lennon, Ahmad A. Elesber, Jeffrey G. Meyer, and Peter B. Berger. “Association of Lipoprotein-Associated Phospholipase A2 Levels with Coronary Artery Disease Risk Factors, Angiographic Coronary Artery Disease, and Major Adverse Events at Follow-Up.” European Heart Journal 26, no. 2 (January 1, 2005): 137–44. https://doi.org/10.1093/eurheartj/ehi010.
“Dietary Goals for the United States / Prepared by the Staff of the Select Committee on Nutrition and Human Needs, United States Senate.,” n.d., 131.
Heyman, Miriam, Jeff Dill, and Robert Douglas. “The Ruderman White Paper On,” n.d., 41.
National Law Enforcement Officers Memorial Fund. “Https://Nleomf.Org/.” Accessed December 21, 2020. https://nleomf.org/.
Kokkinos, Peter. “Physical Activity, Health Benefits, and Mortality Risk.” ISRN Cardiology 2012 (October 30, 2012): 1–14. https://doi.org/10.5402/2012/718789.
Lima João A.C., Desai Milind Y., Steen Henning, Warren William P., Gautam Sandeep, and Lai Shenghan. “Statin-Induced Cholesterol Lowering and Plaque Regression After 6 Months of Magnetic Resonance Imaging–Monitored Therapy.” Circulation 110, no. 16 (October 19, 2004): 2336–41. https://doi.org/10.1161/01.CIR.0000145170.22652.51.
null null, Thom Thomas, Haase Nancy, Rosamond Wayne, Howard Virginia J., Rumsfeld John, Manolio Teri, et al. “Heart Disease and Stroke Statistics—2006 Update.” Circulation 113, no. 6 (February 14, 2006): e85–151. https://doi.org/10.1161/CIRCULATIONAHA.105.171600.
“Parker v. District of Columbia, 850 F.2d 708 | Casetext Search + Citator.” Accessed December 24, 2020. https://casetext.com/case/parker-v-district-of-columbia-2.
Pinizzotto, Anthony, Edward Davis, and Charles Miller III. “The Deadly Mix. Officers, Offenders and the Circumstances That Bring Them Together.” The FBI Law Enforcement Bulletin, January 2007.
Pontzer, Herman, Ramon Durazo-Arvizu, Lara R. Dugas, Jacob Plange-Rhule, Pascal Bovet, Terrence E. Forrester, Estelle V. Lambert, Richard S. Cooper, Dale A. Schoeller, and Amy Luke. “Constrained Total Energy Expenditure and Metabolic Adaptation to Physical Activity in Adult Humans.” Current Biology 26, no. 3 (February 8, 2016): 410–17. https://doi.org/10.1016/j.cub.2015.12.046.
Publishing, Harvard Health. “Surviving a Heart Attack: A Success Story.” Harvard Health. Accessed December 21, 2020. https://www.health.harvard.edu/heart-health/surviving-a-heart-attack-a-success-story.
Ruiz-Ramie, Jonathan J., Jacob L. Barber, and Mark A. Sarzynski. “Effects of Exercise on HDL Functionality.” Current Opinion in Lipidology 30, no. 1 (February 2019): 16–23. https://doi.org/10.1097/MOL.0000000000000568.
Sacks, Frank M., George A. Bray, Vincent J. Carey, Steven R. Smith, Donna H. Ryan, Stephen D. Anton, Katherine McManus, et al. “Comparison of Weight-Loss Diets with Different Compositions of Fat, Protein, and Carbohydrates.” New England Journal of Medicine 360, no. 9 (February 26, 2009): 859–73. https://doi.org/10.1056/NEJMoa0804748.
Sheinberg, Jonathan. “The Presence of Early Markers of Coroanry Artery Disease in an Asymptomatic Population of Law Enforcement Officers,” June 2020.
Shell, Daniel. “The Police Executive Leadership Program Class Exercise and Nutrition Questionnaire, Division of Public Safety Leadership.” Johns Hopkins University, October 2003.
Swift, Damon L., Neil M. Johannsen, Carl J. Lavie, Conrad P. Earnest, and Timothy S. Church. “The Role of Exercise and Physical Activity in Weight Loss and Maintenance.” Progress in Cardiovascular Diseases 56, no. 4 (2014): 441–47. https://doi.org/10.1016/j.pcad.2013.09.012.
“The Officer Down Memorial Page (ODMP).” Accessed December 21, 2020. https://www.odmp.org/.
Tracy, Tom. “Fit for Duty: Demand It.” Police, March 1993, 18.
Varvarigou, Vasileia, Andrea Farioli, Maria Korre, Sho Sato, Issa J. Dahabreh, and Stefanos N. Kales. “Law Enforcement Duties and Sudden Cardiac Death among Police Officers in United States: Case Distribution Study.” BMJ (Clinical Research Ed.) 349 (November 18, 2014): g6534. https://doi.org/10.1136/bmj.g6534.
Violanti, John M., Tara A. Hartley, Ja K. Gu, Desta Fekedulegn, Michael E. Andrew, and Cecil M. Burchfiel. “Life Expectancy in Police Officers: A Comparison with the U.S. General Population.” International Journal of Emergency Mental Health 15, no. 4 (2013): 217–28.
Yokoyama, Mitsuhiro, Hideki Origasa, Masunori Matsuzaki, Yuji Matsuzawa, Yasushi Saito, Yuichi Ishikawa, Shinichi Oikawa, et al. “Effects of Eicosapentaenoic Acid on Major Coronary Events in Hypercholesterolaemic Patients (JELIS): A Randomised Open-Label, Blinded Endpoint Analysis.” The Lancet 369, no. 9567 (March 31, 2007): 1090–98. https://doi.org/10.1016/S0140-6736(07)60527-3.

